Carpal Tunnel Syndrome
-
Anatomy
-
Diagnosis/ Condition
-
Surgical treatment
-
How to lead CPT code
-
CPT code selection criteria
-
Live chart sample
1.Anatomy
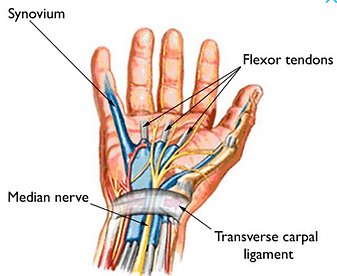
Carpal tunnel as the name something related to Carpal location and that belong to wrist. So carpal tunnel is the narrow passageway surrounding by carpal bone and ligament on the palm side of the hand. Medial nerve is one of the major peripheral nerves of the upper limb than passages through this carpal tunnel.
2.Disease and Condition
Carpal Tunnel Syndrome is the compression of the medial nerves that causing pain, numbness, and tingling.
3.Surgical treatment of carpal tunnel syndrome
-
Carpal Tunnel Release: It is the releasing of the pressure by cutting the transverse carpal tunnel ligament.
-
Carpal Tunnel Injection: The physician injects a steroid in the connect tissue in the carpel tunnel which relieve pressure on the medial nerves. Steroid are anti-inflammatory medicine.
4.How to lead correct CPT Code
In CPT book ,go to carpal tunnel, you will get the code for injection and release.
Carpal Tunnel- Injection, Thermapy- 20526
Carpal Tunnel- Syndrome, Decompression- 64721
Unlisted Cpt for Carpal Tunnel release via Percutaneous or Manos Sytem- 64999
5.Code selection criteria for carpal tunnel syndrome
The code selection criteria for carpal tunnel syndrome
Method of treatment :
1.Decompression
Approach - Open / Endoscopy /Percutaneous
2.Nerves Block
Injection of anesthetic agent
LIVE SAMPLE CHART 2 PREOPERATIVE DIAGNOSIS: CPREOPERATIVE DIAGNOSIS: Right carpal tunnel syndrome. POSTOPERATIVE DIAGNOSIS: Right carpal tunnel syndrome. TITLE OF THE PROCEDURE: Right carpal tunnel release. COMPLICATIONS: There were no complications during the procedure. SPECIMEN: The specimen was sent to pathology. INSTRUMENTS: All counts were correct at the end of the case and no complications were encountered. INDICATIONS: This is a 69-year-old female who have been complaining of right hand pain, which was steadily getting worse over a prolonged period of time. The patient had tried nonoperative therapy, which did not assist the patient. The patient had previous diagnosis of carpal tunnel and EMG showed compression of the right median nerve. As a result of these findings, the patient was sent to my office presenting with this history and was carefully evaluated. On initial evaluation, the patient had the symptomology of carpal tunnel syndrome. The patient at the time had the risks, benefits, and alternatives thoroughly explained to her. All questions were answered. No guarantees were given. The patient had agreed to the surgical procedure and the postoperative rehabilitation as needed. DETAILS OF THE PROCEDURE: The patient was brought to the operating room, placed supine on the operating room table, prepped and draped in the sterile fashion and was given sedation. The patient was then given sedation. Once this was complete, the area overlying the carpal ligament was carefully injected with 1% lidocaine with epinephrine. The patient had this area carefully and thoroughly injected with approximately 10 mL of lidocaine with epinephrine and once this was complete, a 15-blade knife was then used to incise the skin opposite the radial aspect of the fourth ray. Careful dissection under direct visualization was performed through the subcutaneous fat as well as through the palmar fascia. A Weitlaner retractor was then used to retract the skin and careful dissection through the palmar fascia would then revealed the transverse carpal ligament. This was then carefully incised using a 15-blade knife and once entry was again into the carpal canal, a Freer elevator was then inserted and under direct visualization, the carpal ligament was then released. The transverse carpal ligament was carefully released first in the distal direction until palmar fat could be visualized and by palpation no further ligament could be felt. The area was well hemostased with the 1% lidocaine with epinephrine and both proximal and distal dissection along the nerve was performed. Visualization of the transverse carpal ligament was maintained with Weitlaner retractor as well as centric. Both the centric and the Ragnell were used to retract both proximal and distal corners of the incision and the entirety of the area was under direct visualization at all times. Palmar fascia was released both proximally and distally as well as the transverse carpal ligament. Direct palpation of the carpal canal demonstrated a full and complete release. Observation of the median nerve revealed an area of hyperemia in the distal two-thirds of the nerve, which demonstrated the likely area of compression. Once this was complete, hemostasis was established using bipolar cautery and some small surface bleeders and irrigation of the area was performed and then the closure was achieved with 4-0 chromic suture in a horizontal mattress and interrupted stitch. Xeroform was then applied to the incision. A bulky dressing was then applied consisting of Kerlix and Ace wrap, and the patient was taken to the recovery room in stable condition without any complications.
LIVE SAMPLE CHART 3 PREOPERATIVE DIAGNOSIS: Bilateral carpal tunnel syndrome. POSTOPERATIVE DIAGNOSIS: Bilateral carpal tunnel syndrome. PROCEDURES: 1. Right open carpal tunnel release. 64721-RT 2. Cortisone injection, left carpal tunnel. 20526-LT ANESTHESIA: General LMA. ESTIMATED BLOOD LOSS: Minimal. COMPLICATIONS: None. INDICATIONS: This patient is a 50-year-old male with bilateral carpal tunnel syndrome, which is measured out as severe. He is scheduled for the above-mentioned procedures. The planned procedures were discussed with the patient including the associated risks. The risks included but are not limited to bleeding, infection, nerve damage, failure to heal, possible need for reoperation, possible recurrence, or any associated risk of the anesthesia. He voiced understanding and agreed to proceed as planned. DESCRIPTION OF PROCEDURE: The patient was identified in the holding area and correct operative site was identified by the surgeon's mark. Informed consent was obtained. The patient was then brought to the operating room and transferred to the operating table in supine position. Time-out was then performed at which point the surgeon, nursing staff, and anesthesia staff all confirmed the correct identification. After adequate general LMA anesthesia was obtained, a well-padded tourniquet was placed on the patient's right upper arm. The right upper extremity was then prepped and draped in the usual sterile fashion. Planned skin incision was marked along the base of the patient's right palm. Right upper extremity was then exsanguinated using Esmarch. The tourniquet was then inflated to 250 mmHg. Skin incision was then made and dissection was carried down with scalpel to the level of the palmar fascia which was sharply divided by the skin incision. Bleeding points were identified with electrocautery using bipolar electrocautery. Retractors were then placed to allow visualization of the distal extent of the transverse carpal ligament, and this was then divided longitudinally under direct vision. Baby Metzenbaum scissors were used to dissect distal to this area to confirm the absence of any remaining crossing obstructing fibrous band. Retractors were then replaced proximally to allow visualization of proximal extent of the transverse carpal ligament and the release was continued proximally until complete release was performed. This was confirmed by visually and palpably. Next, baby Metzenbaum scissors were used to dissect anteroposterior adjacent antebrachial fascia, and this was divided longitudinally under direct vision using baby Metzenbaum scissors to a level of approximately 3 cm proximal to the proximal extent of the skin incision. Carpal canal was then inspected. The median nerve was flattened and injected. No other abnormalities were noted. Wounds were then irrigated with normal saline and antibiotic additive. Decadron 4 mg was then placed adjacent to the median nerve. Skin incision was then closed with interrupted 5-0 nylon suture. The wound was then dressed with Adaptic, 4 x 4s, Kling, and Coban. The tourniquet was then deflated. Attention was then directed to the left side. Using sterile technique, the left carpal canal was injected with a mixture of 40 mg of Depo-Medrol, 1 cc of 1% lidocaine, and 1 cc of 0.25% Marcaine. Band-Aid was then placed over the injection site. The patient was then awakened, extubated, and transferred over to his hospital bed. He was transported to recovery room in stable condition. There were no intraoperative or immediate postoperative complications. All counts were reported as correct.
LIVE SAMPLE CHART 4 PREOPERATIVE DIAGNOSIS: Bilateral carpal tunnel syndrome. POSTOPERATIVE DIAGNOSIS: Bilateral carpal tunnel syndrome. PROCEDURE PERFORMED: Carpal tunnel release. INDICATIONS FOR SURGERY: Nerve conduction study tests diagnostic of carpal tunnel syndrome. The patient failed to improve satisfactorily on conservative care, including anti-inflammatory medications and night splints. PROCEDURE: The patient was brought to the operating room and, following a Bier block to the operative arm, the arm was prepped and draped in the usual manner. Utilizing an incision that was laid out to extend not more distally than the thumb web space or proximally to a position short of crossing the most prominent base of the palm and in line with the longitudinal base of the thenar eminence in line with the fourth ray, the soft tissue dissection was carried down sharply through the skin and subcutaneous fat to the transverse carpal ligament. It was identified at its distal edge. Using a hemostat to probe the carpal tunnel, sharp dissection utilizing scalpel and iris scissors were used to release the carpal tunnel from a distal-to-proximal direction in its entirety. The canal was probed with a small finger to verify no evidence of any bone prominences. The nerve was examined for any irregularity. There was slight hyperemia of the nerve and a slight hourglass deformity. Following an irrigation, the skin was approximated using interrupted simple and horizontal mattress #5 nylon suture. A sterile dressing was applied. The patient was taken to the recovery room in satisfactory condition.